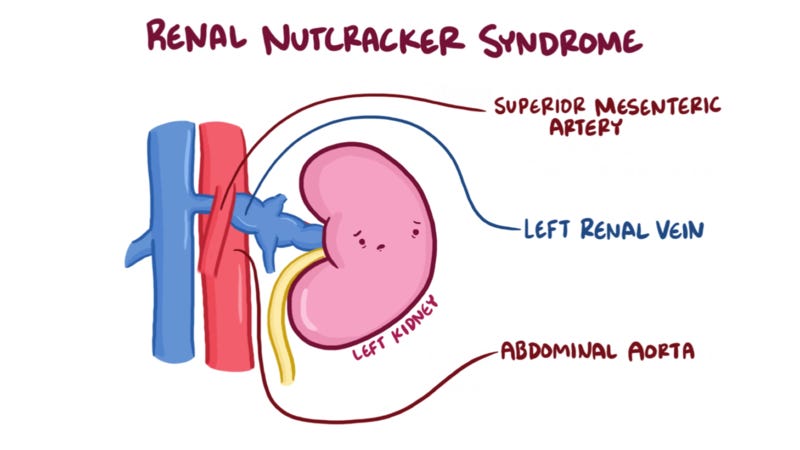
Nutcracker Syndrome (NCS) is a vascular compression syndrome that occurs when the left renal vein is compressed between the superior mesenteric artery and the aorta, leading to a range of symptoms associated with renal vascular congestion. This compression, both anteriorly and posteriorly, can result in complications such as hematuria (blood in urine), orthostatic hypotension, pain, and even renal dysfunction.
There are different forms of NCS, with the classic anterior NCS being the most common. A less frequent variant, Posterior NCS, involves compression between the vertebral column and aorta. Combined NCS has also been reported. Diagnosing NCS is challenging and often involves a combination of approaches. Treatment can vary and is determined on an individual basis, often requiring care from experienced experts in the field.
Symptoms of Nutcracker Syndrome:
Flank Pain: Unexplained pain on one side of the lower back.
Hematuria: Presence of blood in the urine.
Orthostatic Intolerance: Difficulty standing for prolonged periods.
Abdominal Pain: Discomfort in the abdominal region.
Orthostatic Proteinuria: Elevated protein in the urine when standing.
Varicocele: Enlarged veins within the scrotum.
Tachycardia: Abnormally fast heart rate.
Diagnostic Approaches:
CT Angiogram: a CT scan with an injection of dye to image of blood vessels
Doppler Ultrasound: Real-time visualization of blood flow providing anatomical and physiological insights
MRI: Imaging of anatomical structures and compression.
Venogram: X-ray of veins with contrast dye, invasive venography and pressure measurement is often required for definitive diagnosis
Treatments:
Not all cases of nutcracker syndrome require intervention, but when they do, the following treatment approaches may be considered:
Stenting: Laparoscopic placement of an extravascular stent to relieve compression and improve blood flow, alleviating symptoms associated with venous congestion
Kidney autotransplant: surgical removal of the affected kidney, addressing compression issues, and re-implanting the kidney in a new location, often the pelvic area
Vein transposition: repositioning the left renal vein to relieve compression
Barriers to Diagnosis
Diagnosing NCS is challenging due to a lack of defined diagnostic criteria, overlapping symptoms with other disorders, and limited awareness among the medical community.
One publication on nutcracker syndrome suggested that another barrier to diagnosis is that the answer appears too simple - “the mechanical effect of “compression = squeezing” may seem to be a rather too simplistic reason for symptoms or explanation of such a complex pathology in comparison to sophisticated neuro - gastrointestinal explanations” and later stated “standing in an upright position requires that that part of the body between the thorax and the hips (the “belt” region) is stable. Individuals affected by hEDS or HSD are often highly flexible and have a weak core and instability at the spine. CS may in part be a consequence of this instability (authors' opinion), and more readily demonstrated in the upright position.”.
Due to these barriers, patients may struggle to get diagnosed or have to travel to seek care from knowledgeable providers.
Nutcracker Syndrome and EDS:
The connection between Nutcracker Syndrome and connective tissue disorders is beginning to be recognized. Emerging evidence in a few publications suggests a link between NCS and EDS. However, the underlying mechanism is unclear. Individuals with EDS, may be at an increased risk of developing NCS due to inherent weaknesses in their connective tissues and lack of structural support. One study stated, “The authors believe that, due to hyperelasticity and altered collagen, mobility of the viscera occurred, allowing unusual compression of the LRV by the portal vein that in turn led to the reappearance of intense pain, a characteristic symptom of NCS.” about a particular case study. It is also important to note that multiple vascular compression syndromes may also co-occur in EDS patients (such as NCS with MALS and/or SMAS)
Nutcracker Syndrome, though rare, presents a complex set of challenges for both patients and healthcare providers. Increased awareness, improved diagnostic criteria, and collaborative efforts within the medical, patient, and research communities are essential to improving our understanding of NCS and its relationship to EDS.
About special guest, Sydney Severance:
Sydney Severance is a 19-year-old who lives with hEDS and multiple comorbid conditions including SMAS. Her medical journey has fueled her passion for advocacy efforts as she aims to give a voice to people with chronic illnesses. She is a biology major at the College of Charleston will a goal of becoming a gastroenterologist specializing in the GI manifestations of connective tissue disorders. Connecting to a broader purpose, particularly helping future generations with EDS and SMAS, gives Sydney hope. You can follow Sydney on Instagram @OperationUpright.
References
Amato ACM, da Silva AEC, Bernal IM, de Oliveira JC, Di Paschoal Almeida Ribeiro M, Schinzari PS, Dos Santos RV. Combined Nutcracker and Ehlers-Danlos Syndromes: A Case Report. EJVES Vasc Forum. 2020 Feb 27;47:12-17. doi: 10.1016/j.ejvsvf.2020.02.005. PMID: 33078146; PMCID: PMC7287400.
Sandmann W, Scholbach T, Verginis K. Surgical treatment of abdominal compression syndromes: The significance of hypermobility-related disorders. Am J Med Genet C Semin Med Genet. 2021 Dec;187(4):570-578. doi: 10.1002/ajmg.c.31949. Epub 2021 Nov 7. PMID: 34747562.
Kolber MK, Cui Z, Chen CK, Habibollahi P, Kalva SP. Nutcracker syndrome: diagnosis and therapy. Cardiovasc Diagn Ther. 2021 Oct;11(5):1140-1149. doi: 10.21037/cdt-20-160. PMID: 34815965; PMCID: PMC8569268.
Penfold, D. (2022, December 3). Nutcracker syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK559189/
Stubberud, A., Cheema, S., Tronvik, E., & Matharu, M. (2020, August). Nutcracker syndrome mimicking new daily persistent headache: A case report. Cephalalgia : an international journal of headache.
Skeik N, Gloviczki P, Macedo TA. Posterior nutcracker syndrome. Vasc Endovascular Surg. 2011 Nov;45(8):749-55. doi: 10.1177/1538574411419376. Epub 2011 Sep 2. PMID: 21890560.
Reed NR, Kalra M, Bower TC, Vrtiska TJ, Ricotta JJ 2nd, Gloviczki P. Left renal vein transposition for nutcracker syndrome. J Vasc Surg. 2009 Feb;49(2):386-93; discussion 393-4. doi: 10.1016/j.jvs.2008.09.051. PMID: 19216958.