Superior Mesenteric Artery Syndrome (SMAS)
Causes, Symptoms, Treatments, and Connective Tissue with Special Guest, Sydney Severance
Superior Mesenteric Artery Syndrome (SMAS) is a rare vascular compression disorder that affects the third portion of the duodenum, leading to a range of distressing symptoms. From abdominal pain and nausea to unintentional weight loss, SMAS poses significant challenges to those diagnosed. With special guest, Sydney Severance, I’m excited to talk about SMAS, exploring its causes, symptoms, diagnostics, treatments, and the overlap it shares with connective tissue diseases like Ehlers-Danlos Syndrome (EDS).
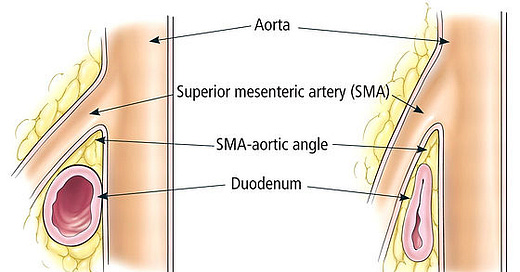
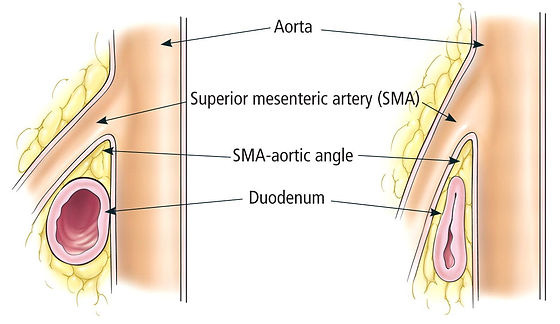
SMAS occurs when the third portion of the duodenum becomes compressed between the abdominal aorta and the superior mesenteric artery, resulting in a range of symptoms such as abdominal pain, nausea, vomiting, early satiety, unintentional weight loss, and bloating.
Diagnostic Approaches
Diagnosing SMAS can be a complex process, often requiring a combination of tests such as:
Upper Gastrointestinal Series
Computed Tomography Angiography (CTA)*
Magnetic Resonance Imaging
Abdominal Ultrasound with Doppler
Hypotonic Duodenography
Barium Swallow Test
*The current CTA criteria involve measuring the aortomesenteric angle and distance, with values below specific thresholds indicating the presence of SMAS.
Treatment Options
The management of SMAS involves both conservative and surgical interventions. Conservative measures include weight gain, nasogastric decompression, and tube feeding beyond the compression site. Surgical interventions may include procedures like duodenojejunostomy and gastrojejunostomy, aimed at relieving the compression and restoring normal digestive function.
Etiology
Understanding the causes of SMAS is crucial for effective management. Etiological factors include the loss of the mesenteric fat pad, thin body build, exaggerated lumbar lordosis, visceroptosis, abdominal wall laxity, and corrective spinal surgery.
The Overlap with Connective Tissue Diseases
Individuals with hypermobile Ehlers–Danlos syndrome (hEDS) or hypermobility spectrum disorder (HSD) may experience nausea, vomiting, and abdominal and pelvic pain, often radiating into the groin and back. Additionally, autonomic dysfunction and neurogastrointestinal issues can occur. These symptoms can be present in a variety of comorbidities associated with EDS and can be difficult to narrow down causes, especially when multiple conditions may be contributing to symptoms. Compression syndromes such as SMAS, median arcuate ligament syndrome (MALS), nutcracker syndrome (NCS), and May–Thurner syndrome (MTS) are often seen in individuals with hypermobility disorders like hEDS. Due the complex nature of these conditions, the diagnostic journey can be long and challenging and may include potential misdiagnoses. One study identified hyperlordosis (excessive inward curvature of lower back), as a factor in the etiology of abdominal, retroperitoneal, and pelvic compression syndromes, particularly in hypermobile individuals.
The exact relationship between compression syndromes like SMAS and connective tissue disorders is not clear. Some possible explanations include:
Connective laxity or weakness impacting structural integrity
Hypermobility in the spine or other anatomical structures could potentially
Weakness in the muscles supporting organs or blood vessel, or muscle imbalances
Genetic factors/genetic predisposition (If certain genes are involved in the development of both EDS and compression syndromes)
Or, maybe a combination of several of these factors.
However, more research is needed to understand casual relationships between these conditions. One recent publication emphasized this relationship, stating “This possible association of SMA and Nutcracker syndrome with Ehlers-Danlos syndrome (EDS) has also been described, so this triad should be considered in other similarly presenting tall, overly flexible patients.”
Superior Mesenteric Artery Syndrome (SMAS) presents a unique set of challenges for both patients and healthcare professionals. As we continue to unravel the pathophysiology surrounding this vascular compression disorder, the potential overlap with connective tissue diseases like EDS will be an important research area. Ongoing research is essential to bridge the gaps in our knowledge and pave the way for more effective diagnostic and treatment strategies for those affected by SMAS and related conditions.
About special guest, Sydney Severance:
Sydney Severance is a 19-year-old who lives with hEDS and multiple comorbid conditions including SMAS. Her medical journey has fueled her passion for advocacy efforts as she aims to give a voice to people with chronic illnesses. She is a biology major at the College of Charleston will a goal of becoming a gastroenterologist specializing in the GI manifestations of connective tissue disorders. Connecting to a broader purpose, particularly helping future generations with EDS and SMAS, gives Sydney hope. You can follow Sydney on Instagram @OperationUpright.
References and Resources:
The SMAS awareness website is an excellent resource for those wanting to learn more! www.smasyndrome.org
Frederick Merrill Karrer, MD. “Superior Mesenteric Artery (SMA) Syndrome.” Practice Essentials, Pathophysiology, Etiology, Medscape, 10 Jan. 2024, emedicine.medscape.com/article/932220-overview#a7.
“Superior Mesenteric Artery Syndrome - about the Disease.” Genetic and Rare Diseases Information Center, U.S. Department of Health and Human Services, rarediseases.info.nih.gov/diseases/7712/superior-mesenteric-artery-syndrome. Accessed 26 Jan. 2024.
Bernotavičius, Giedrius, et al. “Superior Mesenteric Artery Syndrome.” Acta Medica Lituanica, U.S. National Library of Medicine, 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5287987/.
Kim, Ju Young, et al. “Incidence and Risk Factors Associated with Superior Mesenteric Artery Syndrome Following Surgical Correction of Scoliosis.” Asian Spine Journal, U.S. National Library of Medicine, June 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC2857491/.
Sandmann W, Scholbach T, Verginis K. Surgical treatment of abdominal compression syndromes: The significance of hypermobility-related disorders. Am J Med Genet C Semin Med Genet. 2021 Dec;187(4):570-578. doi: 10.1002/ajmg.c.31949. Epub 2021 Nov 7. PMID: 34747562.
England J, Li N. Superior mesenteric artery syndrome: A review of the literature. J Am Coll Emerg Physicians Open. 2021 Jun 18;2(3):e12454. doi: 10.1002/emp2.12454. PMID: 34179879; PMCID: PMC8212557.
Poster Presentation: https://www.jvascsurg.org/article/S0741-5214(22)00873-4/fulltext#articleInformation
Amato ACM, da Silva AEC, Bernal IM, de Oliveira JC, Di Paschoal Almeida Ribeiro M, Schinzari PS, Dos Santos RV. Combined Nutcracker and Ehlers-Danlos Syndromes: A Case Report. EJVES Vasc Forum. 2020 Feb 27;47:12-17. doi: 10.1016/j.ejvsvf.2020.02.005. PMID: 33078146; PMCID: PMC7287400.