Gaps in EDS Medical Education
How education of healthcare providers is failing patients with connective tissue diseases
Whether they know it or not, nearly every healthcare professional will come across Ehlers-Danlos syndrome patients (EDS) in their career. In this blog, joined by Amy Weintraub, we're diving into the lesser-known truths about EDS and dispelling some outdated myths that persist in medical and health professional education.
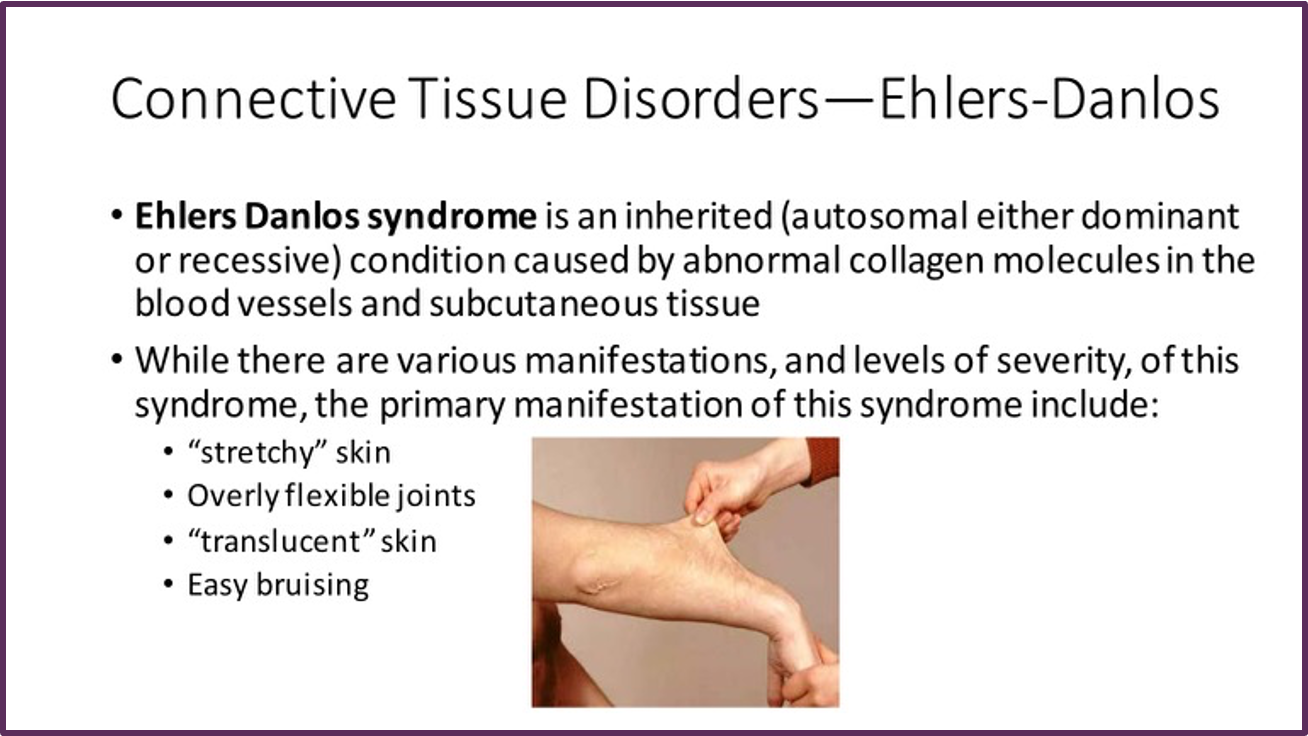
In health professional training, education related to connective tissue disorders and EDS is limited, often consisting of one side with an oversimplification. If mentioned at all, lectures tend to misrepresent EDS, calling it a rare disease (despite recent prevalence estimates of hEDS at 1 in 500), and focus on seemingly benign symptoms of the skin and joints.
The reality of EDS is much more complex. This group of connective tissue disorders comprises 14 subtypes, affecting multiple bodily systems—skin, joints, gastrointestinal, cardiovascular, immunological, and neurological. Manifestations occur on a spectrum, ranging from joint issues and stretchy skin to severe neurological impacts, gastrointestinal paralysis, autonomic dysfunction, and relentless chronic pain.
Accurate diagnosis and informed caregivers are pivotal in managing EDS. Approaches involve diverse strategies in physical therapy, medication, mobility aids, feeding tubes, and possibly surgical procedures, aiming to manage symptoms.
However, individuals with EDS often experience significant delays in diagnosis post-symptom onset. This delay is influenced by inadequate clinical awareness and a failure to implement diagnostic criteria in clinical or genetic diagnoses. Medical education's portrayal of EDS as a 'rare disease,' especially in hEDS, leads physicians to believe they are unlikely to encounter such cases.
Inadequate education and awareness of EDS contribute to diagnostic delays, impacting patients' quality of life. The prevalent "think of horses, not zebras" adage further discourages in-depth investigations into less common diagnoses, potentially overlooking crucial health concerns.
Recent survey studies, such as the 2022 report from Children’s Mercy, unveil the stark lack of comfort among healthcare providers in diagnosing and managing EDS. Only a small percentage felt confident in executing their treatment plans for EDS patients. Surprisingly, while most respondents claimed familiarity with EDS, their comfort level in handling cases remained abysmally low.

Insufficient information taught in medical curricula creates a generalized perception of EDS. It fails to delve into its numerous subtypes and the associated health implications beyond 'excessively flexible joints' and 'elastic skin.' Hypermobility, often deemed benign, can significantly impact various bodily systems. Teaching the misconception that EDS is rare and relatively harmless can be detrimental to both patients and medical professionals.
Recent publications have also highlighted the demand from the patient community in improved education and EDS-focused patient care centers to manage the complex multidisciplinary nature of the disease. In one survey, 49% of patients responded that they were dissatisfied with current care, mentioning “a lack of understanding of EDS and HSD was seen as a critical barrier to getting appropriate care”. Another study mentioned, “Barriers to care for hEDS/HSD patients include limited primary care education and overburdened genetic practices.”. The same publication also cites one of the hurdles as a lack of an accredited specialty training curriculum for EDS.
Another publication highlights healthcare education gaps citing the following key points, “Clinical heterogeneity, common comorbidities, and lack of awareness of HSD and EDS among healthcare providers contribute to underdiagnosis, as many clinical findings can be attributed to other diagnoses without identification of the entire spectrum of symptoms arising from HSD or EDS” and that patients have poor healthcare experiences due to lack of awareness among providers and frequently being ignored or belittled by providers due to misconceptions about EDS.
Equipping Healthcare Providers
Recognizing the need for enhanced knowledge, there are resources available for healthcare professionals. Programs like EDS ECHO and EDS CME Physician Education offer crucial insights into classifying, treating, and diagnosing EDS. Additionally, specific CME journals, like those co-authored by Linda Bluestein, MD and Victoria Daylor on pain and hypermobility, provide valuable insights.
By fostering a deeper understanding of EDS among healthcare providers, we strive for swifter diagnoses, improved care pathways, and enhanced quality of life for individuals living with EDS.
Resources for Healthcare Providers:
EDS ECHO Program: Provides interdisciplinary courses for healthcare professionals caring for EDS/HSD patients.
EDS CME Physician Education Program: Free accredited program offering a comprehensive understanding of EDS.
Pain & Hypermobility CME: A pain management CME on symptomatic joint hypermobility.
More Education Crucial
While healthcare education has made some progress, we still have a long way to go.
We want to hear from you - Please let us know in the comments if there are any other educational gaps you’ve noticed as patients or providers.
More about special guest, Amy Weintraub: Amy recently graduated from the University of South Carolina in December with a degree in Mass Communications. Public Health has always been an interest of hers but since her initial hEDS diagnosis, she has developed a growing interest in science and health communications. Amy hopes to use the personal knowledge she has gained throughout her medical journey along with her love for content creation to spread awareness and advocate for others dealing with complex conditions. You can follow her on Instagram at @amyrosaliee.