Neurological Manifestations of EDS
There is a lot to talk about with EDS when it comes to the brain, spine and nervous system!
When you think of the Ehlers-Danlos Syndromes (EDS), most people tend to think of the joints, skin, and maybe the heart being impacted. But connective tissue is everywhere - and consequences and comorbidities of EDS can extend to neurological symptoms and manifestations.
Spinal Manifestations
Like other joints in the body, ligament laxity of the spine can result in hypermobility and instability.
Spinal instability can affect various regions, including the upper (Atlantoaxial Instability - AAI, and Craniocervical Instability - CCI) middle (thoracic) and lower (lumbar) spine. Detecting spinal instabilities is best done with weight-bearing, dynamic imaging (if you are curious about literature mentioning upright MRI, I recommend these two publications - one and two).
Spinal deformities such as kyphosis and scoliosis may be present (and are more prevalent in rare types of EDS such as kyphoscoliotic EDS). Additional spinal manifestations may include disc degeneration (often a consequence of instability), radiculopathy, myelopathy, and, Tarlov cysts.
The Brain and Spinal Cord
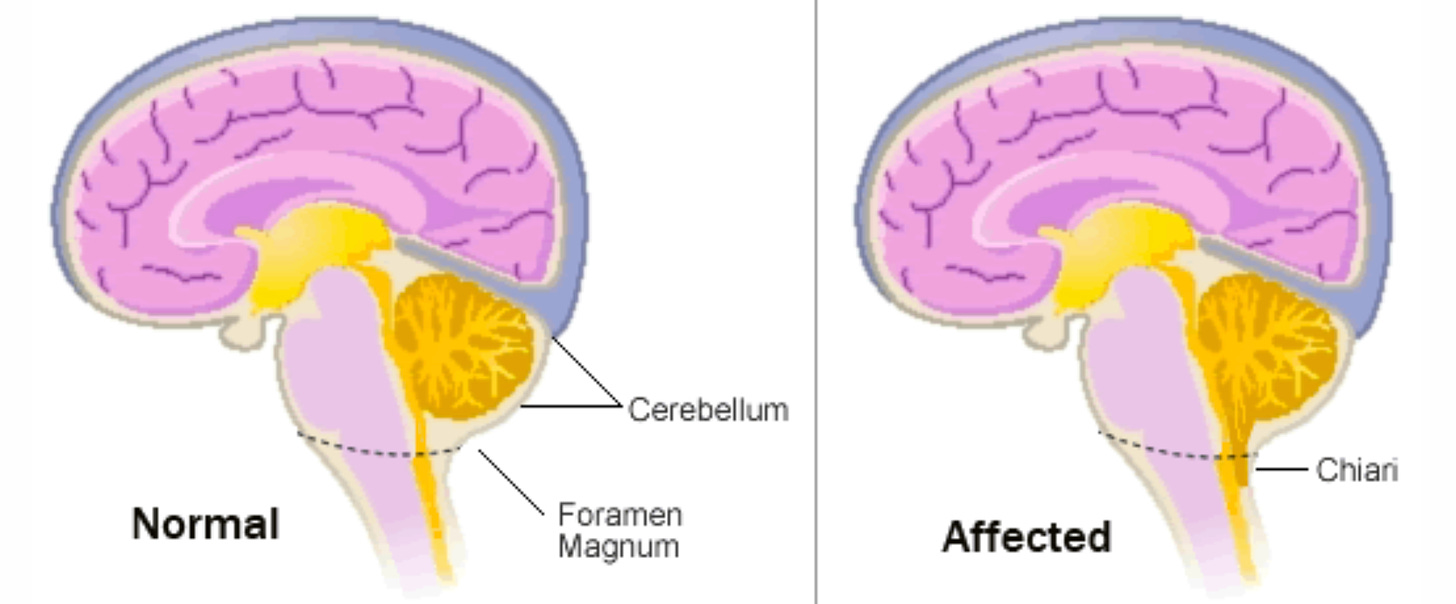
Chiari malformation may occur in EDS patients (the cerebellum, lower part of the brain, extends into the spinal canal). Chiari may be associated with co-occurring CCI or syringomyelia.
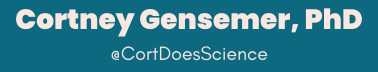
Also gaining more recognition in the EDS space is Tethered cord syndrome (TCS). TCS may be present in EDS due to abnormalities in filum, and is often occult (meaning not detectable on MRI imaging).
Another area of more recent attention is the co-existence of cerebral venous outflow (idiopathic intracranial hypertension (IIH) and associated cerebral venous outflow disorders like CSF leak) and EDS in recently published studies. Spontaneous CSF leak can occur in some patients and may be difficult to diagnose.
Headaches, Pain and Neuropathy
Headaches and migraine are common occurrences for EDS patients. It may be challenging to determine the cause of headaches in EDS patients due to the many neurological comorbidities that can cause them.
Neuropathic pain may happen in EDS patients for a variety of reasons. In some cases, this can be due to conditions such as small fiber neuropathy, nerve entrapments, and other neuralgias. In recent years, studies have highlighted an overlap of small fiber neuropathy in EDS, with one study reporting changes in small nerve fibers in as many as 71% of hEDS patients. Occipital and trigeminal neuralgia are seen in people with EDS and can be a cause of headaches in this population. Sometimes, these neuralgias are thought to be related to underlying upper cervical spine instability, but not in all cases.
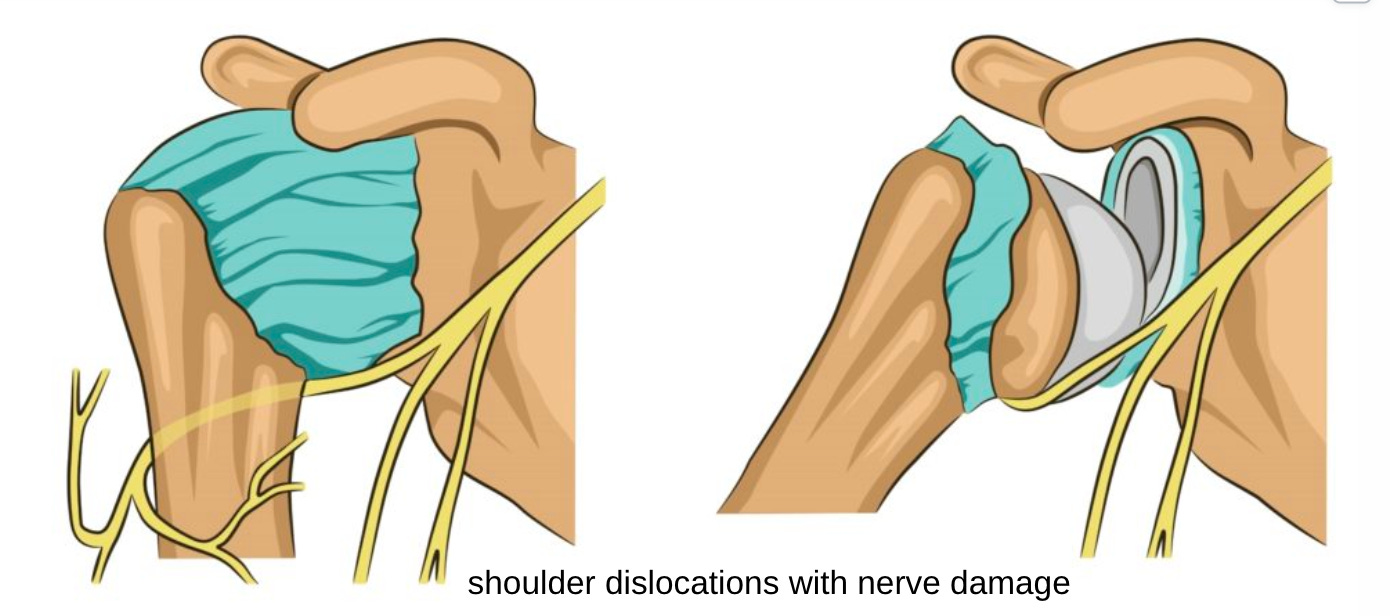
Brachial plexopathies and sciatic neuropathies have been reported and may be a consequence of chronic stretch injury or instability. Dislocations and subluxations may stretch or apply pressure to peripheral nerves resulting in neuropathy or plexopathy.
Autonomic Dysfunction
Another condition that is neurological in nature is dysautonomia or postural orthostatic tachycardia syndrome (POTS). While many people consider POTS in the context of cardiology due to its effects on the vascular system, the underlying cause is dysfunction of the autonomic nervous system and it should also be highlighted as a neuro-comorbidity in this context!
Rare Subtypes of EDS
While most of these neurological manifestations have been studied in the context of hypermobile EDS (hEDS), they may also occur in other subtypes. Unfortunately, a lot of data in other subtypes is limited due to their rarity. In vascular EDS (vEDS) there is an increased risk of stroke and cerebrovascular disease, this risk may also be elevated in other rare types of EDS with vascular fragility. This can include intracranial aneurysm, subarachnoid hemorrhage, spontaneous arterial dissection and cavernous sinus fistula. Kyphoscoliotic EDS (kEDS) is associated with progressive kyphoscoliosis (kyphosis and scoliosis).
These are not the only neurological manifestations that can occur in EDS patients, but just some of the main conditions frequently seen in this population. I look forward to sharing more detailed posts on these topics soon!
Want to stay up to date on the latest literature? Become a paid subscriber to get regular of the latest research and more bonus blogs (including access to all old posts)!
References and Resources:
Castori M, Voermans NC. Neurological manifestations of Ehlers-Danlos syndrome(s): A review. Iran J Neurol. 2014 Oct 6;13(4):190-208. PMID: 25632331; PMCID: PMC4300794.
Gensemer C, Burks R, Kautz S, Judge DP, Lavallee M, Norris RA. Hypermobile Ehlers-Danlos syndromes: Complex phenotypes, challenging diagnoses, and poorly understood causes. Dev Dyn. 2021 Mar;250(3):318-344. doi: 10.1002/dvdy.220. Epub 2020 Aug 17. PMID: 32629534; PMCID: PMC7785693.
https://www.ehlers-danlos.com/2017-eds-classification-non-experts/neurological-spinal-manifestations-ehlers-danlos-syndromes/
Fernandez A, Aubry-Rozier B, Vautey M, Berna C, Suter MR. Small fiber neuropathy in hypermobile Ehlers Danlos syndrome/hypermobility spectrum disorder. J Intern Med. 2022 Dec;292(6):957-960. doi: 10.1111/joim.13539. Epub 2022 Jul 15. PMID: 35781355; PMCID: PMC9796626.
Midtlien JP, Curry BP, Chang E, Kiritsis NR, Aldridge JB, Fargen KM. Characterizing a new clinical phenotype: the co-existence of cerebral venous outflow and connective tissue disorders. Front Neurol. 2024 Jan 10;14:1305972. doi: 10.3389/fneur.2023.1305972. PMID: 38269002; PMCID: PMC10806170.
Henderson FC, Sr., Austin C, Benzel E, Bolognese P, Ellenbogen R, Francomano CA, Ireton C, Klinge P, Koby M, Long D, Patel S, Singman EL, Voermans NC. Neurological and spinal manifestations of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):195-211. Epub 20170221. doi: 10.1002/ajmg.c.31549. PubMed PMID: 28220607.
Marathe N, Lohkamp L-N, Fehlings MG. Spinal manifestations of Ehlers-Danlos syndrome: a scoping review. Journal of Neurosurgery: Spine. 2022:1-11. doi: 10.3171/2022.6.SPINE211011.
Michelini G, Corridore A, Torlone S, Bruno F, Marsecano C, Capasso R, Caranci F, Barile A, Masciocchi C, Splendiani A. Dynamic MRI in the evaluation of the spine: state of the art. Acta Biomed. 2018 Jan 19;89(1-S):89-101. doi: 10.23750/abm.v89i1-S.7012. PMID: 29350639; PMCID: PMC6179074.




Did you know that they’re studying the use of the GLP1 injectables to treat Intracranial Hypertension and having success?