Disclaimer: This blog post is for informational purposes only and does not constitute medical advice. Please consult with a healthcare professional for personalized recommendations and care.
In September 2024, the American Heart Association released a new scientific statement titled Cardiovascular Management of Aortopathy in Children. This document provides a comprehensive framework for managing aortic conditions in pediatric patients, emphasizing the importance of a multidisciplinary approach and personalized care.
Understanding Aortopathy
Aortopathy refers to conditions that lead to issues such as dilation, aneurysm, dissection, or rupture of the aorta and other blood vessels. These conditions may impact the thoracic aorta in children and can be caused by factors such as a bicuspid aortic valve, connective tissue disorders, or heritable (genetic) thoracic aortic diseases. Genetic testing plays a critical role in both diagnosing and guiding the medical management of these conditions. The statement highlights the need for early diagnosis and careful surveillance of aortic conditions in children, particularly those with genetic predispositions.
The Need for Multidisciplinary Care
Aortic conditions in children require more than just cardiovascular management. The AHA recommends multidisciplinary care, involving a range of specialists. Pediatric patients may need input from specialists in genetics, ophthalmology, orthopedics, rehabilitation medicine, physical and occupational therapy, neurology, and more. This approach helps ensure that all aspects of a child's health—especially those affected by connective tissue disorders—are appropriately addressed.
For complex cases, particularly those where the genetic diagnosis is unclear, or escalation in therapy is needed, consultation with a pediatric aortopathy specialist is critical. Managing a child with aortic disease is often not just about treating the heart, but considering the impact of other systems and how they may interact with the condition.
Imaging and Genetic Testing
Imaging is essential for diagnosing and monitoring aortic disease. Transthoracic echocardiograms (TTE) are the primary imaging tool used, but MRI, CT scans, and CTA (especially for evaluating aortic dissection) may also be necessary, depending on the severity of the condition.
The statement highlights that genetic testing allows for better risk stratification and personalized management. If a pathogenic variant is found, genetic testing should be offered to at-risk family members. Conversely, if genetic testing is negative, first-degree relatives should still undergo imaging screening to catch any early signs of aortic disease.
Medication and Exercise Recommendations
Medication plays a role in slowing the progression of aortic disease. Angiotensin receptor blockers (ARBs) and beta-blockers (BBs) are commonly used as they help slow the rate of aortic growth. However, some medications should be avoided, including fluoroquinolone antibiotics and vasoconstricting agents, as they can exacerbate vascular problems.
When it comes to exercise, the statement cautions against high-intensity exertion, as it can raise blood pressure and stress the aortic wall. High-contact sports should also generally be avoided. For children with EDS or hypermobility, special consideration should be given to the potential for joint instability, retinal detachment, and cervical spine issues, as these factors can complicate the management of aortic disease.
Surgical Interventions
In rare cases, aortic dissection can occur in children, and while it’s a rare event, it can be catastrophic. In these instances, surgical intervention becomes essential. Elective replacement of the aortic root and ascending aorta aneurysms is often lifesaving, especially for children with high-risk genetic variants.
For those requiring surgery, experts recommend the involvement of specialized centers to optimize outcomes. Whether the surgery involves a valve-sparing or valve-replacing approach, the expertise of a team skilled in pediatric aortic disease is vital for ensuring the best possible result.
Key Takeaways
Early diagnosis and regular monitoring through imaging, particularly TTE, are essential for evaluating the heart and aorta.
Genetic testing is important for managing heritable thoracic aortic diseases and guiding family care.
Medical management should focus on slowing the progression of aortic disease using ARBs and beta-blockers, while avoiding certain medications.
Surgical interventions should be considered carefully, particularly for high-risk patients, with expert centers playing a key role in optimizing outcomes.
Multidisciplinary care is necessary, addressing all aspects of a child’s health, including non-cardiovascular concerns.
This document provides an invaluable framework for managing aortic disease in children, especially those with underlying connective tissue disorders. If you or your child has a genetic predisposition to aortopathy or is showing signs of cardiovascular issues, I strongly recommend reading the full article and discussing it with your doctor to ensure comprehensive care.
Sharing this scientific statement with your healthcare team can help ensure the best possible management plan tailored to your individual needs, especially when navigating the complexities of pediatric aortopathy and its associated genetic factors.
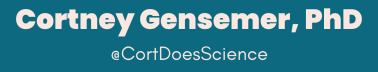
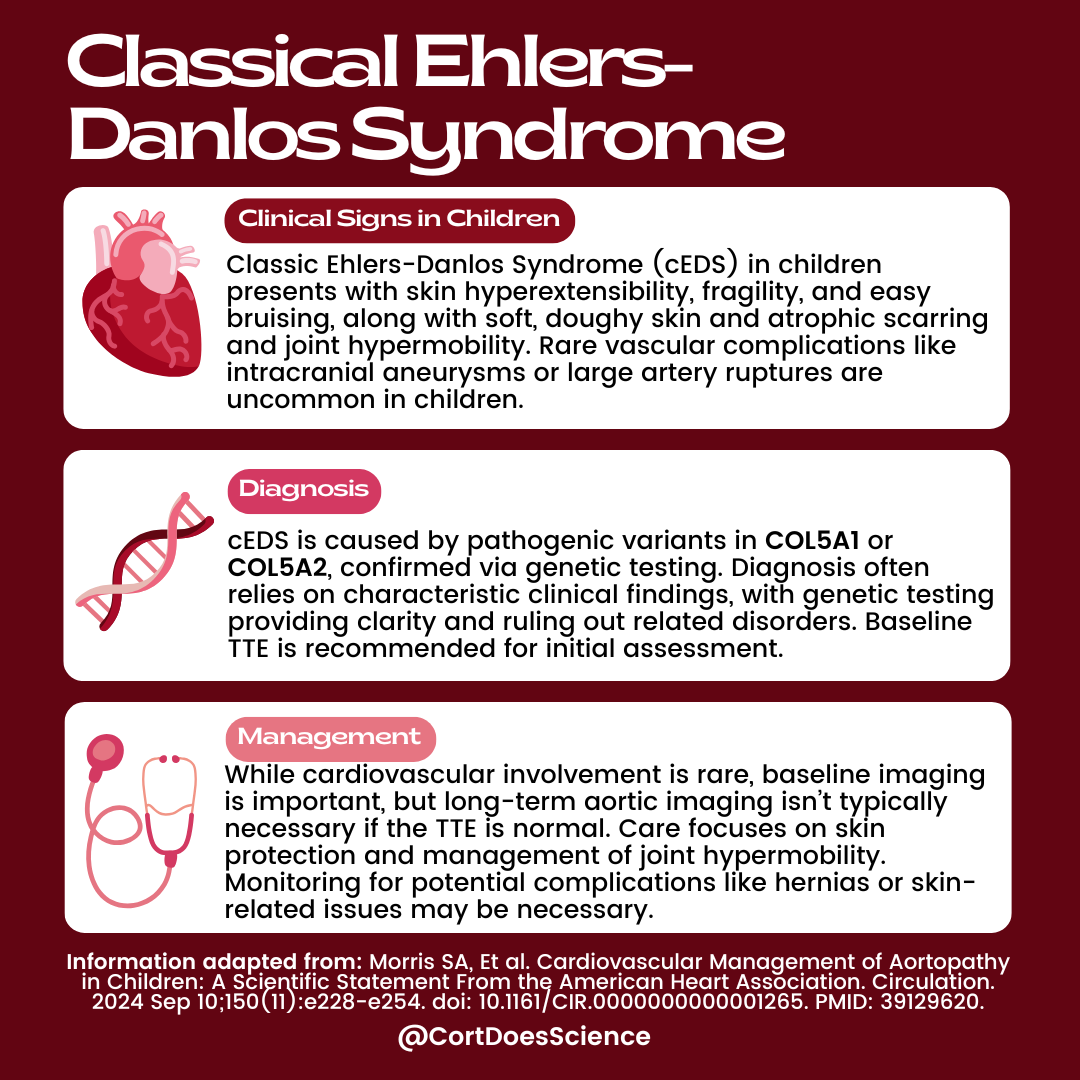
As a brief summary, I created graphics for Marfan Syndrome, Loeys-Dietz Syndrome, Vascular Ehlers-Danlos Syndrome and Classical Ehlers-Danlos Syndrome, however these are not the only conditions mentioned in the report.
You can read the full scientific statement here for a deeper dive into the guidelines and recommendations.
Graphics are always shared on facebook and Instagram too if you ever want to share them on your social media feeds!
Stay up to date with all the latest scientific research by becoming a paid subscriber and getting What’s New In Science (WNIS) in your inbox regularly!