Adrenal Insufficiency Awareness Month: Understanding AI
What is adrenal insufficiency? How is it diagnosed? and where to learn more!
April is adrenal insufficiency (AI) and adrenal disease awareness month. Let’s talk about what AI is and provide resources for those impacted.
What is Adrenal Insufficiency?
Adrenal Insufficiency (AI) is a disorder characterized by the inadequate production of hormones by the adrenal glands. The adrenal glands, situated on top of the kidneys (think kidney hat!), produce crucial hormones such as cortisol, which regulates metabolism and helps the body respond to stress, and aldosterone, which regulates blood pressure. When the adrenal glands fail to produce sufficient amounts of these hormones, it can lead to various symptoms and complications.
(Note: Adrenal Insufficiency is distinct from the popularized notion of "adrenal fatigue," which lacks recognition as a medical condition.)
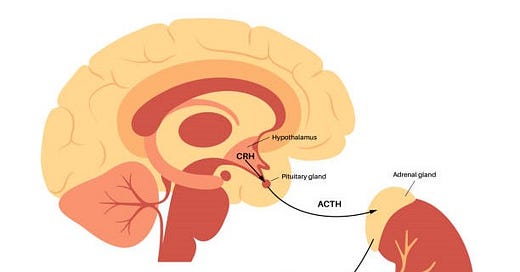
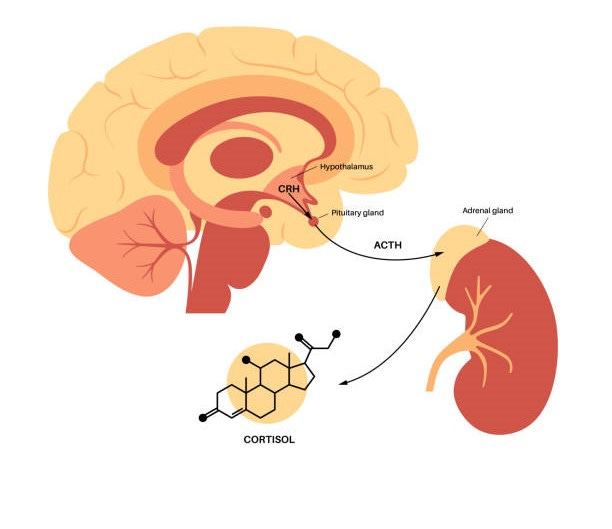
The Hypothalamic-Pituitary-Adrenal (HPA) Axis:
The HPA axis is the body's stress response, regulating hormones through various mechanisms and feedback loops. The hypothalamus, pituitary gland, and adrenal glands are part of the HPA axis regulating the production of cortisol. As a simple overview, not accounting for various feedback loops begins with corticotropin-releasing hormone (CRH) released from the hypothalamus, which then triggers adrenocorticotropic hormone (ACTH) release from the pituitary, finally signaling to the adrenal glands to release cortisol. After cortisol is released from the adrenal glands, it exerts negative feedback on both the pituitary gland and the hypothalamus. This feedback helps regulate cortisol levels within a narrow physiological range.
Disruptions in the HPA axis can lead to adrenal insufficiency resulting in insufficient cortisol production (and the opposite - Cushings syndrome)
Types of Adrenal Insufficiency:
Primary Adrenal Insufficiency (Addison's Disease): Typically autoimmune, Addison's disease can also result from surgical removal of the adrenal glands.
Secondary Adrenal Insufficiency*: The pituitary fails to produce adequate ACTH, essential for stimulating cortisol production.
Tertiary Adrenal Insufficiency*: When insufficient production of CRH leads to reduced cortisol production.
Adrenal insufficiency can also result from prolonged steroid or opioid use, as well as congenital adrenal hyperplasia (CAH), a genetic disorder that can lead to reduced cortisol levels, often overlapping with conditions such as classic-like TNXB Ehlers-Danlos syndrome (clEDS).
*Adrenal insufficiency stemming from the pituitary or hypothalamus is sometimes collectively termed "central adrenal insufficiency."
Symptoms of Adrenal Insufficiency
Adrenal insufficiency presents a diverse array of symptoms, ranging from general malaise to more serious symptoms.
Fatigue and Weakness
Weight Loss
Gastrointestinal Symptoms: Nausea, vomiting, diarrhea and abdominal pain
Darkening of the skin (Addison’s Disease)
Dehydration (Addison’s Disease)
Low blood pressure, dizziness when standing up, fainting (more obvious in Addison’s)
Low-grade fever
Low blood sugar (more common in secondary AI)
Salt craving (Addison’s Disease))
muscle and joint pain
Tremors
Menstrual Irregularities
Hyperkalemia (Addisons Diease)
These symptoms may vary in severity and onset, often becoming more pronounced during periods of stress or illness, such as after a COVID-19 infection (two recent papers: one and two), or following interventions such as treatment for hypothyroidism.
Signs of Adrenal Crisis:
Adrenal crisis is a life-threatening condition characterized by a severe deficiency of cortisol, often precipitated by stress, illness, injury, or abruptly stopping the use of steroid medication.
Some signs of adrenal crisis include:
Sudden Severe Weakness or Fatigue:
Severe Abdominal Pain, nausea and vomiting
Fever
Confusion or Loss of Consciousness
For individuals with known adrenal insufficiency, it's important to carry an emergency injection kit containing hydrocortisone or dexamethasone, along with clear instructions on its administration. In the event of adrenal crisis, prompt administration of the emergency injection can provide the lifesaving cortisol needed to stabilize the individual until medical help arrives.
Chronic symptoms of AI may be present without crisis until patients experience a severe stressor. However, the first (obvious) presentation is often during a crisis.
Diagnosing AI:
The diagnostic process for adrenal insufficiency can require several different tests depending on the type of AI suspected.
Basal Serum Cortisol Testing: Basal serum cortisol levels are measured, typically in the early morning (8AM), to exclude adrenal insufficiency and determine the need for further evaluation. This test should be interpreted alongside clinical assessment. It is often paired with ACTH. This test can rule out AI if levels are over a certain threshold, but for many people may put you in a “grey area” that warrants further testing.
ACTH Stimulation Tests: A standard high-dose ACTH stimulation test involves administering synthetic ACTH and measuring cortisol levels at 30 and 60 minutes post-injection. Interpretation is based on peak cortisol values, with specific thresholds to exclude or diagnose adrenal insufficiency. In primary AI, this test is fairly accurate for diagnosis. In secondary, this test may still be normal.
Metyrapone Stimulation Test: This test involves administering metyrapone, a medication that blocks cortisol synthesis, and measuring the subsequent levels of cortisol and 11-deoxycortisol. Abnormal results may indicate primary or secondary adrenal insufficiency. Further evaluation is needed to distinguish between the two, typically by assessing basal or metyrapone-stimulated plasma ACTH concentrations. The metyrapone test is particularly sensitive for detecting partial defects in pituitary corticotropin secretion, making it valuable in evaluating suspected cases of secondary adrenal insufficiency, especially in the event of low cortisol but normal ACTH stimulation test.
DHEAS Testing: Dehydroepiandrosterone sulfate (DHEAS) levels may be measured, especially when cortisol and ACTH testing results are inconclusive. While low DHEAS levels support the diagnosis of adrenal insufficiency, they are not used as a sole diagnostic tool.
Aldosterone and Renin Testing: Elevated aldosterone levels with low renin activity may suggest primary aldosteronism, while low aldosterone levels with low or high renin activity may indicate adrenal insufficiency.
Antibody Testing for Adrenal Insufficiency: Elevated levels of anti-21-hydroxylase antibodies or other adrenal-specific antibodies may indicate autoimmune adrenal insufficiency, aiding in the diagnosis of conditions such as Addison's disease.
A combination of tests may be run to evaluate for AI and to determine the type of AI for appropriate treatment.
Managing AI:
Managing adrenal insufficiency (AI) primarily involves hormone replacement therapy, typically with corticosteroids such as hydrocortisone, prednisone, or dexamethasone. These medications aim to replace the deficient hormones, particularly cortisol, and are usually taken orally (in a much lower dose than what is given for other health conditions). However, it's important to note that some individuals with Addison's disease may require additional steroids, such as fludrocortisone, to replace aldosterone, which helps regulate blood pressure and electrolyte balance.
Medication adherence is crucial in AI management to maintain stable hormone levels and prevent adrenal crisis, a life-threatening condition resulting from cortisol deficiency. Patients must adhere to their prescribed medication schedule diligently, including taking extra doses during times of illness or stress. Moreover, lifestyle adjustments, such as maintaining a well-balanced diet, staying hydrated, and getting adequate rest, are essential. Stress management techniques, including relaxation exercises, mindfulness practices, and seeking support from healthcare professionals and support groups, can also help individuals with AI better cope with stressors that may exacerbate their condition.
To learn more about adrenal insufficiency, check out the resources below.
Resources and Support:
Resources and support for individuals with adrenal insufficiency are crucial for obtaining reliable information and finding a supportive community. Reputable organizations such as the National Adrenal Diseases Foundation (NADF) and the Addison's Disease Self-Help Group offer valuable resources, including educational materials, guidelines, and updates on research and treatment options. The NADF also lists ongoing clinical trials for patients to enroll in. Online communities and support groups provide a platform for individuals living with adrenal insufficiency to connect, share experiences, and seek advice from peers who understand their challenges firsthand.
References for Further Reading: